Why are scientists trying to manufacture organs in space?
This article was originally published at The Conversation. The publication contributed the article to Space.com's Expert Voices: Op-Ed & Insights.
Alysson R. Muotri, Professor of Pediatrics and Cellular and Molecular Medicine, University of California San Diego
Gravity can be a real downer when you are trying to grow organs.
That’s why experiments in space are so valuable. They have revealed a new perspective into biological sciences, including insights into making human tissues.
Gravity influences cellular behavior by impacting how protein and genes interact inside the cells, creating tissue that is polarized, a fundamental step for natural organ development. Unfortunately, gravity is against us when we try to reproduce complex three dimensional tissues in the lab for medical transplantation. This is difficult because of the intrinsic limitations of bio-reactors used on Earth.
I am a stem cell biologist and interested on brain health and evolution. My lab studies how the human brain is formed inside the womb and how alterations in this process might have lifelong consequences to human behavior, such as in autism or schizophrenia. Part of that work includes growing brain cells in space.
Growing tissue and organs in the lab
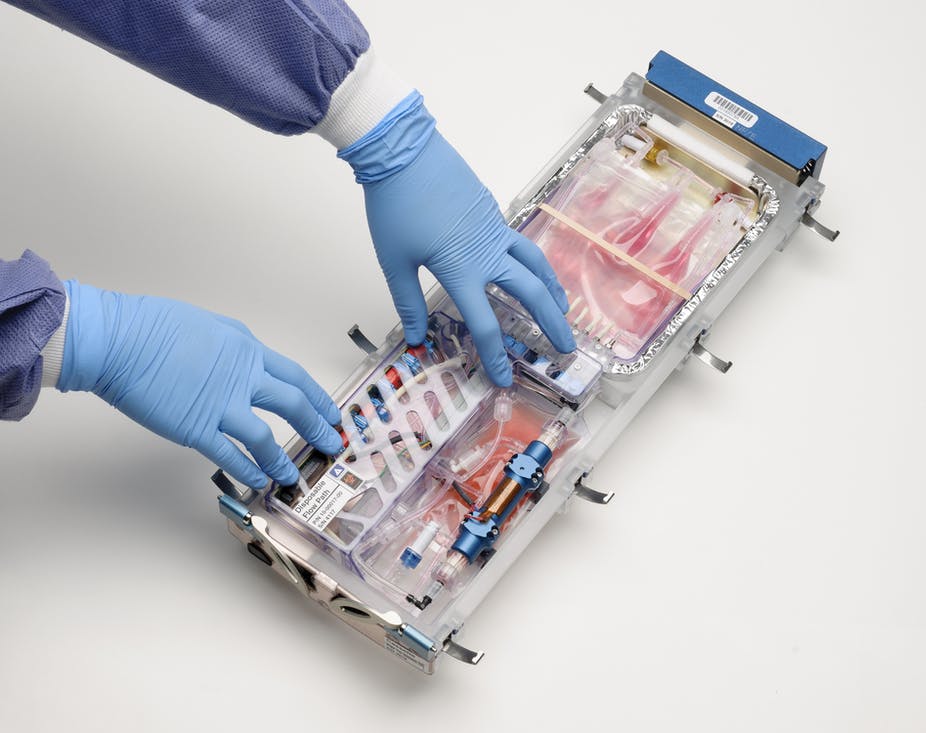
To build organized tissues in the lab, scientists use scaffolds to provide a surface for cells to attach based on a predetermined rigid shape. For example, an artificial kidney needs a structure, or scaffold, of a certain shape for kidney cells to grow on. Indeed, this strategy helps the tissue to organize in the early stages but creates problems in the long run, such as eventual immune reactions to these synthetic scaffolds or inaccurate structures.
Get the Space.com Newsletter
Breaking space news, the latest updates on rocket launches, skywatching events and more!
[Deep knowledge, daily. Sign up for The Conversation’s newsletter.]
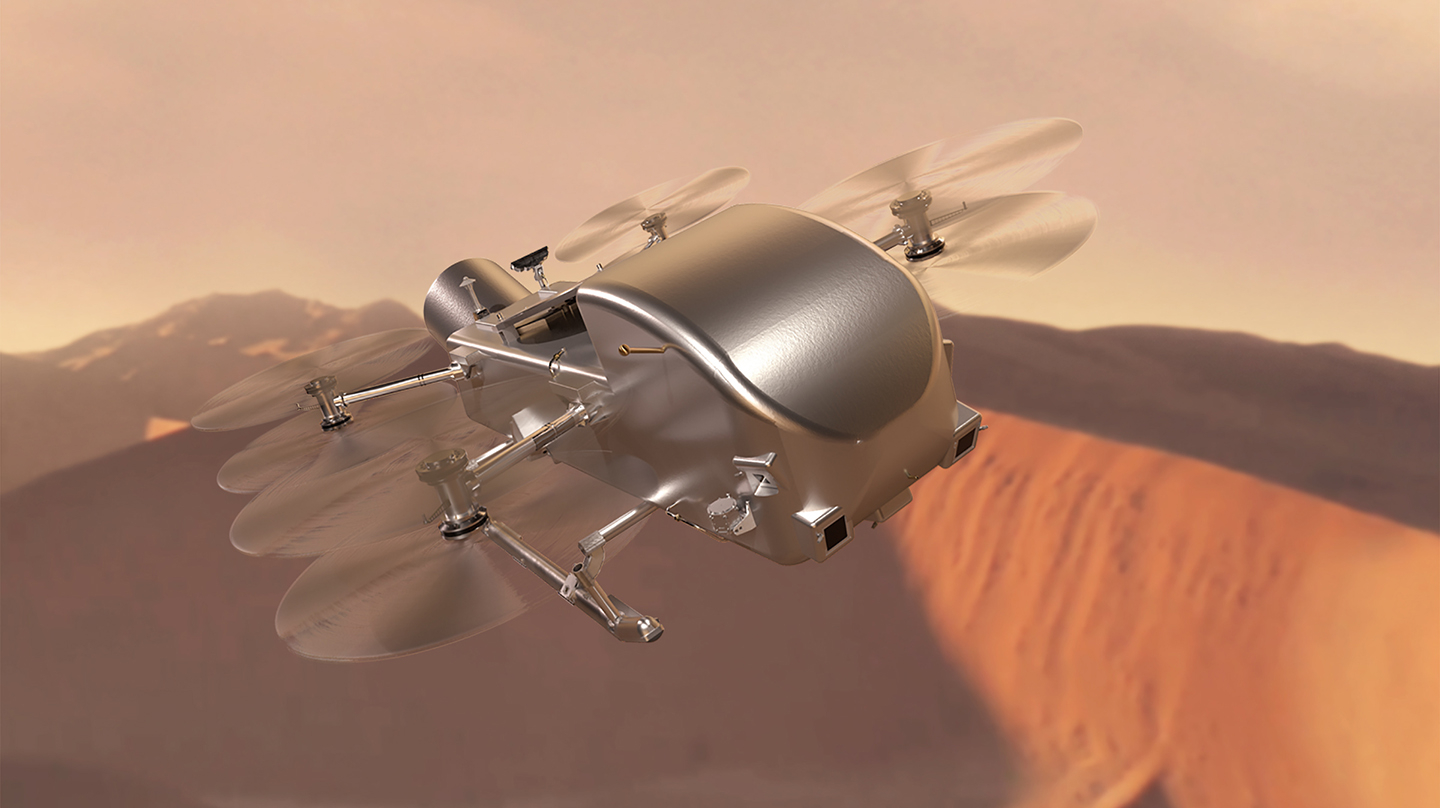
By contrast, in weightless conditions, cells can freely self-organize into their correct three-dimensional structure without the need for a scaffold substrate. By removing gravity from the equation, we researchers might learn new ways of building human tissues, such as cartilage and blood vessels that are scaffold-free, mimicking their natural cellular arrangement in an artificial setting. While this is not exactly what happens in the womb (after all the womb is also subject to gravity), weightless conditions does give us an advantage.
And this is precisely what is happening at the International Space Station.
These experiments help researchers optimize tissue growth for use in basic science, personalized medicine and organ transplantation.
But there are other reasons why we should manufacture organs in space. Long-term space missions create a series of physiological alterations in the body of astronauts. While some of these alterations are reversible with time, others are not, compromising future human spaceflights.
Studying astronauts’ bodies before and after their mission can reveal what goes wrong on their organs, but provides little insights on the mechanisms responsible for the observed alterations. Thus, growing human tissues in space can complement this type of investigation and reveal ways to counteract it.
Finally, all forms of life that we know about have evolved in the presence of microgravity. Without gravity, our brains might have evolved in a different trajectory, or our livers might not filter liquids as it does on Earth.
By recreating embryonic organ formation in space, we can anticipate how the human body in the womb would develop. There are several research initiatives going on in my lab with human brain organoids at ISS, designed to learn the impact of zero gravity on the developing human brain. These projects will have profound implications for future human colonization (can humans successfully reproduce in space?). These studies will also improve the generation of artificial organs that are used for testing drugs and treatments on Earth. Will better treatments for neurodevelopmental and neurodegenerative conditions that affects millions of people come from research in space?
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Follow all of the Expert Voices issues and debates — and become part of the discussion — on Facebook and Twitter. The views expressed are those of the author and do not necessarily reflect the views of the publisher.
Join our Space Forums to keep talking space on the latest missions, night sky and more! And if you have a news tip, correction or comment, let us know at: community@space.com.

Dr. Muotri earned a BSc in Biological Sciences from the State University of Campinas in 1995 and a Ph.D. in Genetics in 2001 from University of Sao Paulo, in Brazil. He moved to the Salk Institute as Pew Latin America Fellow in 2002 for a postdoctoral training in the fields of neuroscience and stem cell biology. He has been a Professor at the School of Medicine, University of California in San Diego since 2008. His research focuses on modeling neurological diseases, such as Autism Spectrum Disorders, using human induced pluripotent stem cells. His lab has developed several techniques to culture human neurons and glia for basic research and drug-screening platforms. He has received several awards, including the prestigious NIH Director’s New Innovator Award, NARSAD, Emerald Foundation Young Investigator Award, Surugadai Award from Tokyo University, Rock Star of Innovation from CONNECT, NIH EUREKA Award among others.